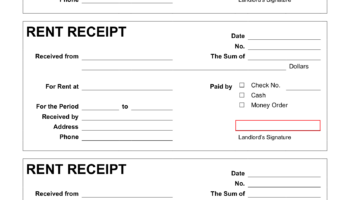
A standardized document facilitating the systematic collection of patient health data is frequently utilized in healthcare settings. This type of document, often formatted for digital accessibility and ease of distribution, enables practitioners to record observations from various body systems. An example includes a multi-page document with clearly labeled sections for vital signs, cardiovascular assessment, neurological evaluation, and musculoskeletal examination. Such forms are typically available for download and subsequent printing to facilitate use during patient encounters.
The availability of such instruments streamlines the process of documentation, promoting consistency across examinations and facilitating effective communication among healthcare providers. These forms provide a structured framework for assessment, ensuring that essential areas are evaluated and documented. The use of these standardized tools can improve patient safety by reducing the likelihood of overlooked findings, and contribute to more efficient record-keeping and better tracking of patient health over time. Historically, paper-based forms were the standard, but modern advancements in digital document formats have enhanced accessibility and ease of integration with electronic health records.
The subsequent sections will delve into the key components of such a form, exploring its practical application, and discussing considerations for its selection and effective implementation within a clinical practice.